November 7, 2025
Explore the many mental-health treatment spaces—from hospital care to therapy offices—and find what healing means for you.
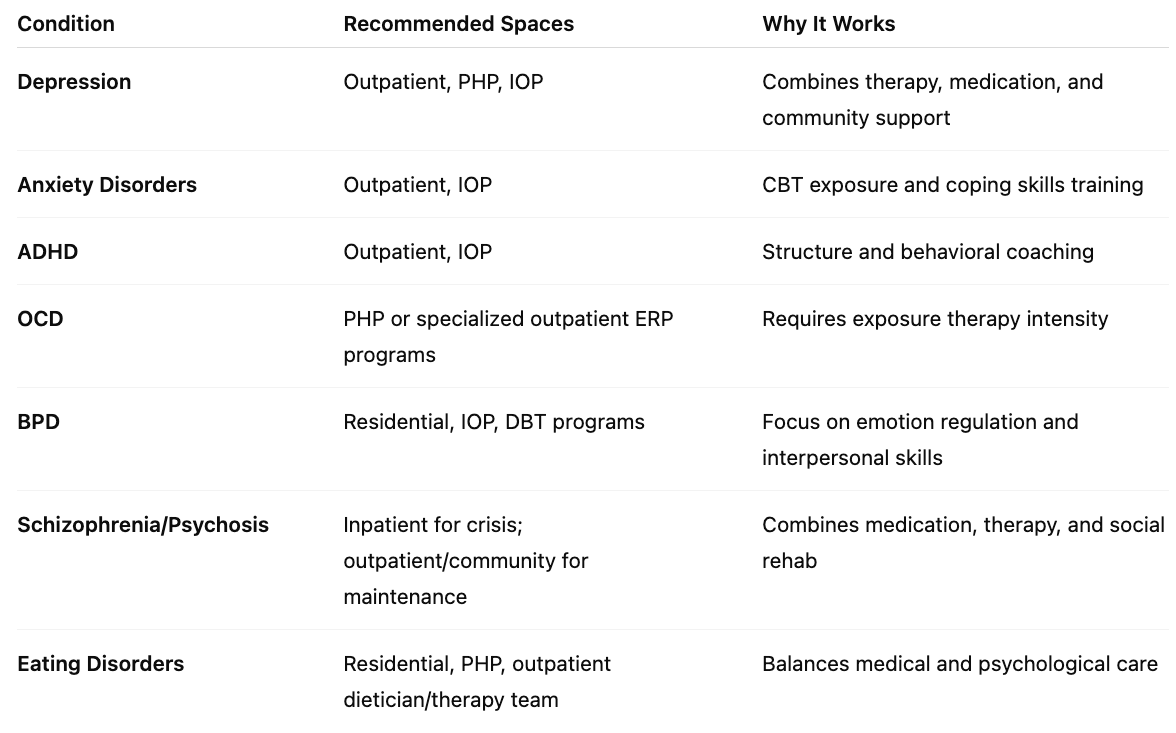
Mental-health treatment isn’t one-size-fits-all. Just as physical medicine has emergency rooms, rehab centers, and clinics, mental-health care happens across different spaces, each designed to meet a unique level of need.
Some people need 24-hour support to stay safe. Others need community connection, structure, or simply a quiet space to talk once a week. Understanding the range of treatment spaces helps remove fear—and stigma—from getting help.
Think of it as a continuum of care, where each step supports the next: from hospital care to outpatient therapy to online support, all forming a safety net for healing.
If someone is in immediate danger—suicidal thoughts, psychosis, severe manic episodes—an inpatient psychiatric hospital offers 24/7 safety and stabilization.
These units aren’t the dark, cold rooms movies depict. They’re structured environments with nurses, psychiatrists, and therapists who help calm crisis and restore balance. Patients might stay anywhere from a few days to a few weeks.
Common conditions treated here:
Once symptoms stabilize, patients often step down to less-intensive settings like partial hospitalization or residential treatment.
Residential programs are like boarding schools for recovery—safe, structured homes that focus on therapy, community, and daily living skills.
Residents might live on-site for 30–90 days, attending therapy, mindfulness groups, and art or movement classes. They cook meals, connect with peers, and rebuild trust in themselves.
Who it helps most:
Residential care offers what daily life often can’t—time and space to rebuild from the inside out.
Imagine spending your day focused entirely on mental wellness—but sleeping in your own bed at night. That’s a Partial Hospitalization Program, or PHP.
Participants attend structured therapy 5 days a week for 4–8 hours daily. It’s often used to prevent hospitalization or help people transition out of it.
A typical day might include:
It’s particularly useful for people with depression, anxiety, OCD, or BPD who need intensive daily support but can function safely at home.
If PHP is “day school,” IOP is “part-time college.” It’s intensive but flexible—3 to 5 days per week, 3 hours at a time.
IOPs are ideal for people returning to work, school, or parenting while continuing to heal. These programs blend group therapy, skills training, and psychiatric follow-ups.
Best for:
An IOP gives structure without removing independence, helping individuals build confidence in managing symptoms while staying connected to their daily lives.
Outpatient therapy is what most people picture when they think of mental-health treatment: weekly or biweekly sessions with a licensed therapist or psychiatrist.
Therapists use approaches like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), or psychodynamic therapy, depending on a person’s needs.
It’s perfect for mild to moderate mental-health concerns—or for maintaining progress after higher-level care.
Commonly treated in outpatient settings:
In outpatient care, healing becomes a part of everyday life, not a pause from it.
Not all therapy happens in clinics. Community-based programs, like clubhouses, drop-in centers, and peer-support groups, are essential spaces for recovery and belonging.
Here, lived experience becomes expertise. Members support one another through empathy and shared understanding. It’s healing through human connection.
Examples:
These spaces can reduce isolation, a major driver of relapse in conditions like depression and psychosis.
Telehealth has made therapy as accessible as your living room. Video sessions, texting therapy, and app-based platforms (like Talkspace or BetterHelp) connect clients and clinicians anywhere, anytime.
Advantages:
Challenges:
When balanced well, telehealth expands access—especially for people who might otherwise avoid therapy due to stigma or logistics.
A good clinician can help evaluate your needs and recommend the right fit. Remember: movement between spaces is normal and healthy. Healing is not linear—it’s adaptive.
Treatment spaces are becoming more inclusive, trauma-informed, and person-centered than ever before.
The future of mental-health treatment is flexible, humane, and deeply personal—meeting people where they are, both emotionally and physically.
If you or someone you know is having thoughts of suicide, hallucinations, or cannot ensure personal safety, seek emergency care immediately.
Call or text 988 (the Suicide & Crisis Lifeline), or go to your nearest emergency department.
At Integrative Psych, we believe that every person deserves the right level of care, at the right time, in the right environment. Our clinicians specialize in guiding clients through every stage of mental-health recovery—from early intervention to ongoing therapy.
Our Chelsea-based team includes psychiatrists, psychologists, and therapists who provide:
Whether you’re exploring therapy for the first time or transitioning from another program, our experts help you navigate your next steps with compassion and clarity.

We're now accepting new patients
