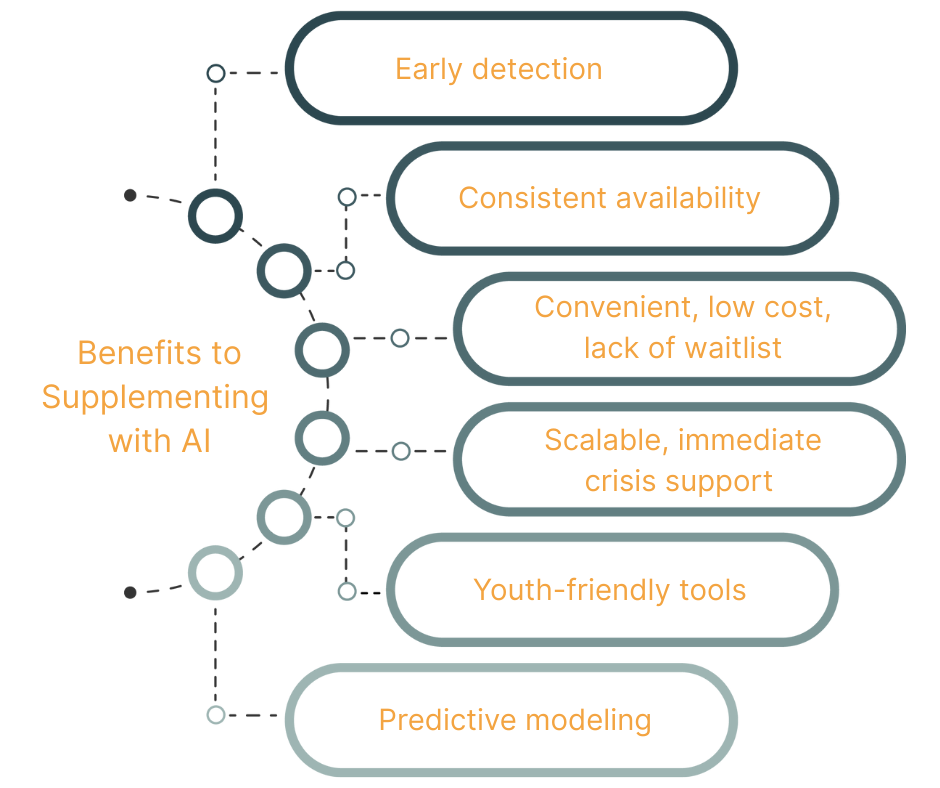
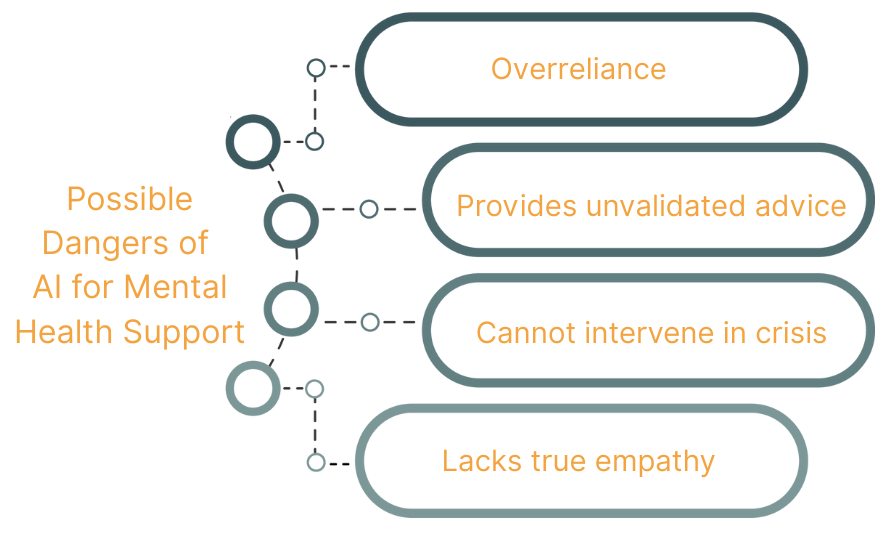
Artificial intelligence is revolutionizing how we live, work, and heal. AI is rapidly transforming mental health by expanding access to support, enhancing clinical insights, and personalizing care—yet it also raises urgent questions about empathy, safety, and the irreplaceable value of human connection.
Natural language processing (NLP) is being used in the Sultan Lab to analyze clinical notes and better understand mental health risks, such as e-cigarette use, to create more informed and personalized treatment plans.
At Integrative Psych, we provide comprehensive, compassionate mental health care in both New York City and Miami, combining cutting-edge innovation with a deeply human approach to healing.


We're accepting new clients.
Book your consultation below.