October 30, 2025
Understand separation anxiety in teens—its signs, causes, and treatments to support healthy emotional growth.
Separation anxiety is commonly associated with young children, but it can also occur—and even intensify—during adolescence. Separation Anxiety Disorder (SAD) in teens involves excessive fear or distress about being apart from parents, caregivers, or significant attachment figures.
While occasional worry about independence or safety is normal during teenage years, separation anxiety becomes a disorder when that fear is persistent, disproportionate, and interferes with daily life—school, socialization, or self-esteem.
According to the National Institute of Mental Health (NIMH), separation anxiety affects roughly 4–5% of children and adolescents, often emerging before age 18. The teenage form can be subtler—expressed through irritability, somatic complaints, or avoidance rather than overt clinginess.
Adolescence is a period of identity formation and emotional volatility. Teens navigate new responsibilities, romantic attachments, academic pressures, and social comparisons—all while developing neurological independence from parents.
However, for some, the developmental drive toward autonomy collides with intense fear of abandonment, rejection, or catastrophe if separated from trusted figures. This fear may reflect unresolved attachment patterns, family stress, or predispositions toward anxiety.
Left untreated, teen separation anxiety can escalate into panic disorder, depression, or generalized anxiety disorder (GAD) in adulthood. Early recognition and intervention are key.
Separation anxiety manifests across emotional, physical, and behavioral domains.
If these symptoms persist for at least four weeks and impair functioning, clinicians may diagnose Separation Anxiety Disorder per DSM-5 criteria.
Separation anxiety in teens rarely stems from a single cause—it reflects a mix of biological, psychological, and environmental influences.
Teens with a family history of anxiety or mood disorders are more prone to developing separation anxiety. Dysregulation of the amygdala (fear center) and prefrontal cortex (emotional regulation) may amplify threat perception.
Highly sensitive or perfectionistic teens—often associated with ADHD or OCD traits—may be more reactive to uncertainty or loss of control.
Overprotective or anxious parenting can unintentionally reinforce fear of independence. Conversely, inconsistent caregiving or early trauma can disrupt trust, leading to anxious attachment.
Divorce, relocation, death of a loved one, or starting a new school can trigger or worsen separation anxiety.
Separation anxiety often co-occurs with:
Adolescence is a period of rapid brain remodeling—particularly in circuits that regulate fear, attachment, and executive function. The amygdala (responsible for detecting threats) and the anterior cingulate cortex (emotional regulation) remain highly active, while the prefrontal cortex (responsible for rational control) matures later.
This developmental gap explains why teens experience emotions intensely but may lack coping mechanisms to manage distress.
Chronic separation stress activates the hypothalamic-pituitary-adrenal (HPA) axis, increasing cortisol. Elevated stress hormones impair sleep, concentration, and immune function—fueling a cycle of anxiety and exhaustion.
Teens may skip school, perform poorly, or struggle with attendance anxiety—especially after weekends or vacations. Teachers often misinterpret these behaviors as defiance rather than distress.
Peers may perceive the anxious teen as “clingy” or immature, increasing risk for bullying or social withdrawal.
Parents, desperate to ease distress, may accommodate avoidance (“Okay, you can stay home today”), inadvertently reinforcing anxiety. Over time, this creates dependency loops that erode autonomy.
Fear of sleeping away from home, going to college, or taking trips reflects deeper worries about separation from emotional anchors.
Adolescents naturally oscillate between independence and dependence. Missing parents during stressful transitions is normal. The distinction lies in degree and impairment.
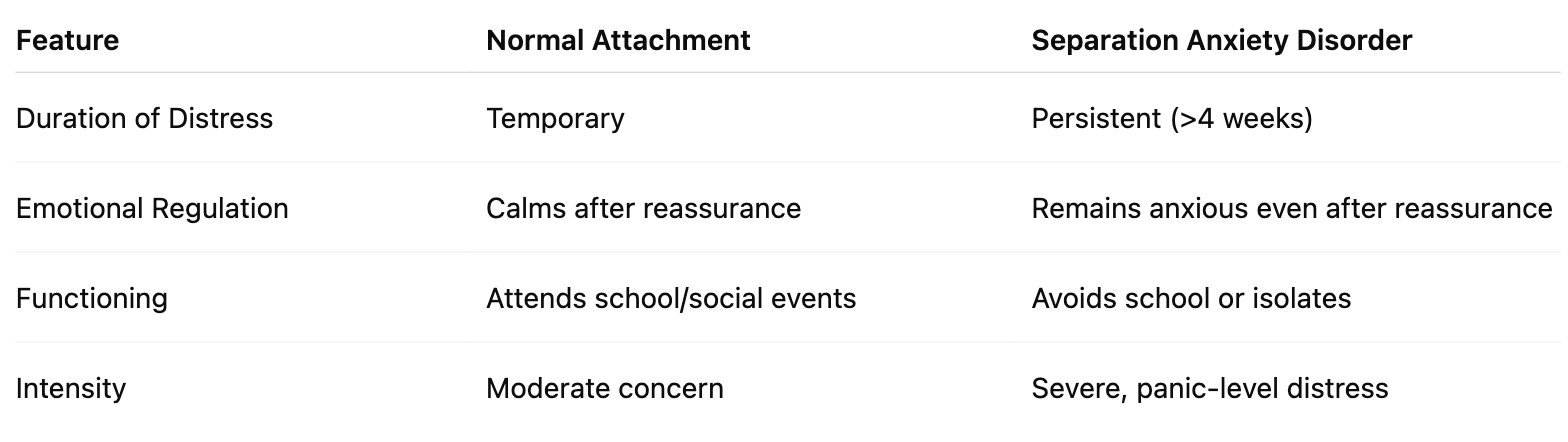
Recognizing these distinctions prevents overpathologizing normal adolescence while ensuring early intervention for true disorder.
Clinicians use structured interviews and standardized tools like:
Differential diagnosis rules out panic disorder, social anxiety, or depression. Assessment often includes family input to capture home-school dynamics.
Effective treatment for teenage separation anxiety blends psychotherapy, family involvement, and lifestyle modification.
CBT helps teens identify catastrophic thoughts (“Something bad will happen”) and replace them with balanced perspectives. Gradual exposure exercises desensitize the fear of being apart from caregivers.
ERP—a subtype of CBT—encourages confronting feared separations without engaging in reassurance or avoidance. Over time, distress decreases naturally.
Parental anxiety and accommodation often perpetuate the problem. Family sessions teach supportive, non-enabling responses—validating feelings while reinforcing independence.
For teens with emotional dysregulation or BPD traits, DBT improves distress tolerance and interpersonal effectiveness, reducing crisis reactions during separation.
Selective Serotonin Reuptake Inhibitors (SSRIs) may be prescribed when psychotherapy alone is insufficient. Pharmacological treatment targets underlying anxiety circuits and helps balance mood.
Counselors can provide safe spaces for check-ins, gradual attendance plans, and coordination with parents to prevent avoidance cycles.
Techniques such as deep breathing, progressive muscle relaxation, and guided imagery reduce physiological arousal and promote calm during separations.
Parents play a crucial role in managing separation anxiety. Key strategies include:
Integrated treatment that addresses both core anxiety and co-occurring conditions yields the best outcomes.
Most teens respond well to early intervention. Prevention involves:
With proper therapy and family collaboration, teens can build confidence, autonomy, and resilience—transforming fear of separation into trust in their own capabilities.
Case: A 15-year-old girl develops intense panic before school after her mother’s hospitalization. She insists on staying home, fears her mother will die, and texts her every hour.
Treatment: CBT with gradual exposure; mother learns to limit reassurance while offering emotional validation.
Outcome: Over three months, panic subsides, school attendance normalizes, and communication patterns become healthier.
At Integrative Psych, our clinicians specialize in supporting teens and families through anxiety, attachment, and emotional growth. We understand that separation anxiety can mask deeper challenges—depression, ADHD, OCD, BPD, or trauma—and that healing requires both empathy and expertise.
Our Chelsea-based team offers:
If your teen struggles with excessive worry, school avoidance, or fear of being apart, help is available.

We're now accepting new patients
