November 14, 2025
Learn the difference between difficult-to-treat depression and treatment-resistant depression and how each is diagnosed and treated.

Depression is one of the most common mental-health conditions globally, yet up to 30–40% of individuals do not fully respond to initial treatment. This has led clinicians to use terms like Treatment-Resistant Depression (TRD) and Difficult-to-Treat Depression (DTD).
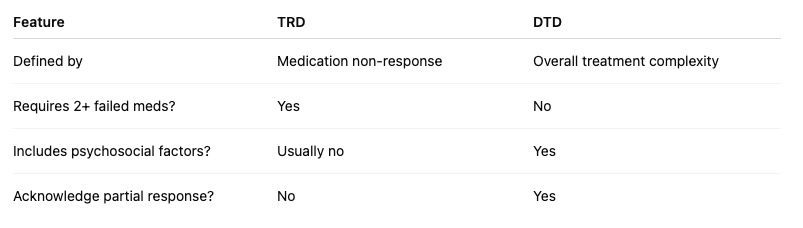
Although these terms are sometimes used interchangeably, they are not the same—and the difference matters for diagnosis, treatment planning, insurance coverage, and patient expectations.
Understanding whether someone has DTD or TRD helps clinicians tailor care more precisely and gives patients a clearer path toward recovery.
Treatment-Resistant Depression (TRD) is a specific clinical designation describing major depression that has not responded adequately to at least two trials of antidepressants, each:
TRD is primarily medication-focused: it reflects pharmacological non-response.
Difficult-to-Treat Depression (DTD) is a broader, more comprehensive term describing depression that continues to cause significant impairment despite ongoing, optimized treatment—but does not require complete medication failure to qualify.
A person may respond partially or intermittently, yet still struggle to maintain remission.
Someone with DTD may:
DTD reflects complexity, not failure.
Depression rarely exists in isolation. Co-occurring disorders profoundly affect treatment response.
Generalized anxiety, panic disorder, and social anxiety often exacerbate depressive symptoms and complicate treatment.
Rumination, rigidity, and perfectionism reduce therapy flexibility and medication response.
Intense mood instability, interpersonal volatility, and abandonment fears interfere with long-term stability—common in DTD.
Depressive symptoms may reflect negative symptoms, medication side effects, or functional decline.
Malnutrition, body-image fear, and compulsive behaviors limit treatment efficacy.
Addressing comorbidities is essential for both DTD and TRD, but particularly DTD, since functional complexity lies at its core.
TRD emphasizes breakthrough; DTD emphasizes management.
Labeling someone as “treatment-resistant” can feel demoralizing.
“Difficult-to-treat” acknowledges complexity, not failure.
DTD treatment is multidimensional:
biological + psychological + relational + lifestyle + context.
Not necessarily.
Both are valid and treatable when addressed with nuance.
At Integrative Psych, we specialize in diagnosing and treating both Treatment-Resistant Depression (TRD) and Difficult-to-Treat Depression (DTD) with a comprehensive, whole-person approach.
Our expert clinicians in Chelsea, NYC and Miami offer:
Whether your depression feels chronic, complicated, or stuck, we’re here to help you move forward with clarity and hope.

We're now accepting new patients
