October 7, 2025
Discover the key differences between CBT vs DBT, two popular mental health therapies. Learn which is best for emotional regulation, ADHD, and more.
Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are popular mental health methods. Both aim to improve emotional well-being and behavior. CBT focuses on changing negative thought patterns. It helps individuals develop healthier ways of thinking and behaving. DBT, a form of CBT, emphasizes acceptance and change. It is particularly effective for emotional regulation and managing intense emotions. These therapies are used to treat various mental health conditions. They include depression, anxiety, and borderline personality disorder. CBT techniques involve cognitive restructuring and problem-solving. DBT skills focus on mindfulness, distress tolerance, and interpersonal effectiveness.
Choosing between CBT and DBT depends on individual needs and goals. Each therapy offers unique benefits and approaches. Understanding the differences can help individuals make informed decisions. It can guide them in selecting the right therapy for their situation. This article will explore the key differences between CBT and DBT. It will provide insights into their applications and effectiveness.
Cognitive Behavioral Therapy (CBT) is a widely used form of behavioral therapy. It is structured and goal-oriented, focusing on changing negative thought patterns. This therapy aims to improve emotional well-being by addressing distorted thinking.
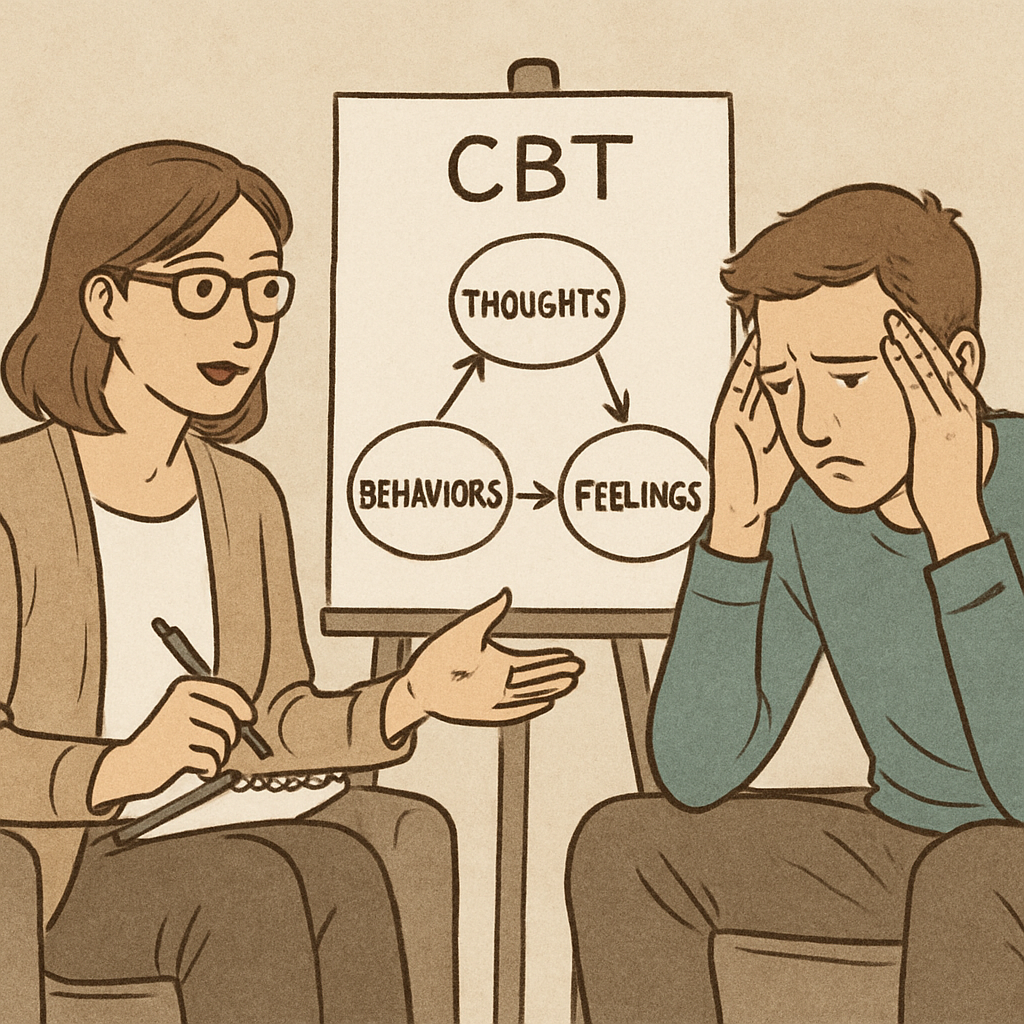
CBT operates on the principle that thoughts, feelings, and behaviors are interconnected. By altering negative thoughts, individuals can influence their emotions and actions. This approach helps clients develop healthier coping mechanisms.
The therapy is highly individualized and often short-term. It typically involves regular sessions with specific objectives. Homework assignments reinforce the skills learned during therapy sessions, promoting real-world application.
CBT is effective for a variety of mental health conditions. These include anxiety, depression, obsessive-compulsive disorder (OCD), and phobias. The therapy's versatility makes it applicable to different populations, including children and adults.
Key components of CBT include:
CBT encourages self-awareness and self-reflection, empowering individuals to take an active role in their recovery.
Dialectical Behavior Therapy (DBT) is a specialized form of cognitive therapy. Initially developed for borderline personality disorder, it now addresses various mental health issues. DBT focuses on balancing acceptance and change for emotional regulation.
The therapy integrates cognitive-behavioral techniques with mindfulness strategies. It helps clients cultivate greater self-awareness and manage intense emotions effectively. DBT promotes the development of practical skills for everyday challenges.
DBT involves both individual and group sessions, unlike traditional CBT. Individual sessions target personal challenges, while group sessions offer skills training and support. This multifaceted approach fosters skill application in real-life situations.
The core components of DBT include:
DBT's emphasis on acceptance helps reduce self-criticism and judgment. It also aids individuals in developing a life worth living, characterized by meaningful goals and relationships.
DBT is especially effective for those struggling with self-harm, suicidal thoughts, and emotional dysregulation. Its comprehensive approach requires dedication and active participation from clients.

Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) share foundational roots but diverge in their core principles. Both aim to foster better mental health through structured, evidence-based methods. However, their approach to change and acceptance varies significantly.
CBT centers on restructuring negative thought patterns to create positive behavior changes. It emphasizes challenging and changing cognitive distortions. By doing so, individuals can improve emotional well-being and behavioral outcomes.
DBT, conversely, integrates acceptance into its practice. It acknowledges that acceptance is as vital as change for emotional growth. This balance helps individuals manage overwhelming emotions more effectively.
Key principles of CBT and DBT include:
While CBT is more direct in confronting negative thoughts, DBT incorporates mindfulness and interpersonal skills. Understanding these principles helps in choosing the most suitable therapy for individual needs. Both approaches provide unique benefits for a range of mental health conditions.
Cognitive Behavioral Therapy (CBT) offers an array of techniques aimed at improving mental health. These techniques are designed to change unhelpful thought patterns and behaviors, which in turn enhance emotional regulation.
One fundamental CBT technique is cognitive restructuring. This involves identifying distorted thinking and replacing it with more balanced thoughts. By doing so, individuals learn to approach situations with clearer perspectives.
Exposure therapy is another critical component, often used for anxiety and phobia treatment. It involves gradual exposure to feared situations to reduce avoidance behaviors. This helps increase confidence and reduce fear over time.
CBT also emphasizes the importance of problem-solving skills. Clients are encouraged to develop strategies to address daily life obstacles effectively. This empowers them to take proactive measures in managing challenges.
Key CBT techniques include:
These techniques, coupled with practical exercises and homework assignments, foster skill application beyond therapy sessions. Through CBT, individuals gain tools to maintain mental health improvements long-term.
Dialectical Behavior Therapy (DBT) equips individuals with critical skills necessary for managing intense emotions and improving interpersonal effectiveness. Originally developed for borderline personality disorder, it is now applied to various mental health conditions.
At the core of DBT is mindfulness, which helps clients develop a heightened awareness of their thoughts and surroundings. This practice promotes living in the present moment without judgment and enhances emotional regulation skills.
Distress tolerance skills are another pivotal component. These skills equip individuals to handle crises without resorting to harmful behaviors. By using techniques like "self-soothing" and "distraction," patients can manage situations without exacerbating them.
Emotion regulation is a vital skill taught in DBT. It helps individuals recognize and alter emotional responses before they become overwhelming. This skill aids in reducing emotional vulnerability and increasing positive emotional experiences.
Key DBT skills include:
These skills are practiced in both group settings and individual sessions, offering varied opportunities to apply what is learned. Regular practice of DBT skills empowers individuals to create a fulfilling and balanced life.
Cognitive Behavioral Therapy (CBT) is renowned for its versatility in addressing numerous mental health disorders. It is frequently employed to treat anxiety disorders, depression, phobias, and obsessive-compulsive disorder (OCD). CBT's structured approach makes it effective for short-term intervention and measurable progress.
On the other hand, Dialectical Behavior Therapy (DBT) initially targeted borderline personality disorder. However, its scope has since broadened. It now benefits individuals with severe emotional regulation issues, self-harm behaviors, and eating disorders. DBT's focus on acceptance and change makes it uniquely suited for long-term therapy.
Both therapies find application in treating post-traumatic stress disorder (PTSD), though with different approaches. CBT often uses exposure and cognitive restructuring techniques, while DBT's mindfulness and distress tolerance are particularly beneficial.
In summary, these therapies are suited for:
Their adaptive methodologies allow therapists to tailor interventions to specific client needs, thereby enhancing therapy outcomes.
When it comes to Attention Deficit Hyperactivity Disorder (ADHD), both CBT and DBT offer distinct advantages. CBT is often the primary choice for managing ADHD due to its structured nature. It helps individuals develop organizational skills and address negative thought patterns that may exacerbate inattention and impulsivity.
DBT, however, excels in providing skills for emotional regulation, which can be beneficial for those with ADHD who experience intense emotions. These skills can improve emotional control and interpersonal effectiveness, enhancing overall functioning.
Beyond ADHD, each therapy shines in other areas. CBT is effective for anxiety and mood disorders. Its focus on cognitive restructuring supports individuals in overcoming depression and anxiety through challenging unhelpful thoughts.
DBT, meanwhile, is particularly beneficial for conditions involving emotional instability. It emphasizes skills like mindfulness, which aid in coping with emotional stressors effectively.
To summarize, the application of these therapies includes:
Selecting between CBT and DBT involves considering specific symptoms and individual therapy goals.
CBT and DBT differ in their therapy formats and delivery methods. CBT typically involves individual therapy sessions. These are often structured around the client's specific goals and involve homework assignments between sessions to reinforce learning.
In contrast, DBT employs a combination of individual and group therapy settings. The inclusion of group sessions allows for the practice of interpersonal skills in a supportive environment. This structure is designed to help clients generalize skills to real-world situations.
Both therapies require a commitment to regular sessions and practice. They incorporate active participation from clients, which is crucial for developing and maintaining the skills learned. Here's a brief look at the delivery format:
Understanding these differences can help in choosing the right therapy approach for personal needs.
CBT, DBT, ACT, and EMDR are all distinct therapeutic approaches. Each is designed to address different mental health needs. While CBT targets changing negative thought patterns, DBT integrates acceptance with change.
ACT, or Acceptance and Commitment Therapy, emphasizes accepting thoughts rather than altering them. It teaches clients to commit to actions aligning with their values. On the other hand, EMDR, or Eye Movement Desensitization and Reprocessing, is primarily used to address trauma and PTSD through guided eye movements.
Understanding the unique features of each therapy helps in making informed choices. Here’s a brief comparison:
Selecting the right therapy involves considering specific symptoms, goals, and preferences.
Deciding between CBT and DBT depends on several factors. Your specific symptoms and personal goals are key elements. Knowing which therapy aligns with these can guide your decision.
Consider the nature of your challenges. CBT might suit those who wish to address distorted thought patterns. If you're struggling with intense emotions or relationships, DBT may provide effective skills.
Individual preferences also play a role. Some may prefer the structured approach of CBT, while others might find DBT’s skills training appealing. Before choosing, it’s crucial to consult with a qualified therapist to evaluate:
Ultimately, understanding these factors ensures that you select a therapy that best supports your journey to better mental health.
Combining CBT and DBT can offer a more holistic approach to therapy. Therapists may blend techniques from both to address unique client needs. Integrating these therapies maximizes strengths while covering a wider range of symptoms.
This combined approach allows clients to benefit from the structured cognitive techniques of CBT. It also offers DBT’s emphasis on emotional regulation. Considerations for integration include:
Together, CBT and DBT can enhance overall treatment outcomes, providing diverse tools for recovery.
CBT focuses on changing negative thought patterns to affect behavior. DBT aims at emotional regulation and acceptance. Each therapy is structured differently to achieve its goals.
Both therapies have proven effective for various conditions. However, therapy effectiveness depends on individual needs and commitment. Considerations include:
Both therapies emphasize active participation, making engagement crucial for success.
Choosing between CBT and DBT depends on your personal needs and goals. Consider the specific symptoms you want to address. If changing negative thinking patterns aligns with your goals, CBT might be beneficial. Conversely, if emotional regulation is your focus, DBT offers useful skills.
Consulting with a mental health professional can provide clarity. They can help tailor the therapy approach to your situation. Remember, both therapies require commitment and active participation for the best outcomes. A strong therapeutic relationship is key to success in any therapy.

We're now accepting new patients
