October 23, 2025
Explore the genetic, environmental, and neurodevelopmental causes of autism spectrum disorder | Integrative Psych
Understanding the causes of autism spectrum disorder is essential for parents, clinicians, educators, and those interested in neurodevelopmental conditions. Although no single cause has been found, research increasingly points to a complex interplay of genetic, biological, and environmental influences. At the same time, individuals with autism spectrum disorder (ASD) often experience comorbid mental-health conditions such as depression and anxiety. This article will explore the major theories on what causes ASD, highlight how it may intersect with other mental-health conditions, and provide practical considerations for families and clinicians.
According to the Autism Spectrum Disorder (ASD) definition by the Mayo Clinic, ASD is a neurodevelopmental condition characterized by challenges in social communication, restricted or repetitive behaviours, and variable strengths and support needs.
Parents often ask, “what causes autism in kids?” The honest answer: there is no single cause. Most researchers agree that autism arises from a combination of inherited genetic variation plus environmental exposures that influence brain development during pregnancy and the first years of life. This view aligns with decades of data on recurrence risk in families, twin studies, and neurodevelopmental biology.
One of the most consistent findings is that genetics plays a major role in ASD risk. Family and twin studies show high heritability estimates. For example, certain gene mutations, copy number variations (CNVs), or inherited genetic variants may raise the likelihood of ASD. However, because no single “autism gene” explains the majority of cases, researchers emphasise a polygenic model, which is many genes each contributing a small risk.
The genetic causes of autism include:
Genetics does not predetermine outcomes. Genes set probabilities, not certainties, and they interact with the environment and developmental timing.
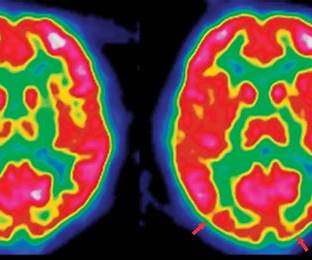
Neurobiological studies suggest differences in brain structure, connectivity, and synaptic communication in ASD. Some research points to disruptions in fronto-striatal circuits, the cerebellum, and sensory integration pathways. These neural differences may contribute to the core features of ASD (social-communication differences, restricted behaviours) and also overlap with findings in other mental-health conditions (e.g., ADHD, OCD).
A central theme is timing: early brain development autism causes emphasize events from conception through toddlerhood. During this window, synapses are formed and pruned, neural circuits are organized, and sensory-social systems take shape. Small shifts—due to genetic variants or exposures—can influence how social communication, sensory processing, and learning unfold, contributing to spectrum-level differences.
“Environment” spans prenatal health, perinatal complications, and early-life factors. Examples frequently studied include advanced parental age, extreme prematurity, maternal infection, certain medications, and air pollution. The field is careful here: most exposures raise risk, not inevitability. It’s more accurate to discuss autism spectrum disorder risk factors than to claim single, linear causes.
While genetics set the stage, environmental and prenatal factors appear to shape risk and expression of ASD. According to the Mayo Clinic, potential contributors include maternal infections, certain medications during pregnancy, air pollution exposure, premature birth, and parental age.
For instance, children born very prematurely (before 26 weeks) or those with certain neurological conditions (such as tuberous sclerosis) show elevated ASD risk.
Recent research emphasises that genes don’t operate in isolation; instead, epigenetic mechanisms (how genes are expressed) may mediate the impact of environmental exposures. For example, prenatal stress or maternal immune activation may interact with a genetic vulnerability to increase ASD risk. However, the science is still emerging and causality is difficult to prove.
Therefore, researchers increasingly describe multifactorial causes autism spectrum disorder to capture the combined effects of:
This framework explains why presentation is so heterogeneous: the mix and timing of influences differ for each person.
A commonly asked question: “Do vaccines cause autism?” The clear research consensus is: no. Despite repeated studies and retraction of the original flawed research, the myth persists and can distract from understanding true risk factors.
Individuals with ASD frequently experience other conditions, and understanding these overlaps is important in both causes and management.
Autistic individuals have higher rates of mood disorders such as Major Depressive Disorder and Generalized Anxiety Disorder. While these conditions may not be “causes” of ASD, the shared neurobiological and psychosocial burdens highlight how mental-health and developmental conditions interconnect.
Autism and ADHD comorbidity is common. Overlapping attentional control, executive function, and arousal regulation pathways may contribute to both conditions. Practical takeaways: assess for ADHD symptoms explicitly, optimize school/work accommodations, and consider behavioral/medication strategies targeting attention and impulsivity.
Repetitive behaviors in autism can resemble compulsions. However, autism spectrum disorder and OCD differ in their drivers: autistic routines often soothe sensory or predictability needs, whereas OCD compulsions aim to neutralize intrusive thoughts. Accurate differentiation guides CBT approaches (including ERP for OCD) and medication planning.
Autism eating disorders comorbidity may involve sensory sensitivities to texture or smell, rigid routines, interoceptive differences, or body-image concerns. Treatment benefits from autism-informed, sensory-aware adaptations to standard eating-disorder protocols, with coordination across therapists, dietitians, and medical providers.
The phrase neurodevelopmental disorders autism schizophrenia overlap reflects shared genetic and neurobiological pathways in some individuals. While schizophrenia and psychosis are distinct diagnoses, overlapping risk architecture suggests a neurodevelopmental continuum. Clinicians should monitor for psychosis risk factors in autistic youth and adults when indicated and use nuanced differential diagnosis.
Though rarer, individuals on the spectrum may experience psychosis or symptoms overlapping with Schizophrenia, or difficulties that resemble borderline personality disorder (BPD). These overlaps urge a neuro-developmental understanding rather than purely psychiatric classification. Some of the same neural circuits and genetic vulnerabilities may be at play.
By exploring these overlaps, we deepen our understanding of how the causes of autism spectrum disorder might also involve broader brain-development pathways that underlie multiple mental-health conditions.
Many risk factors operate during prenatal or early post-natal brain development. Genetic vulnerability plus environmental triggers early in life may shape brain wiring in a way that gives rise to ASD.
The current consensus: there is no single cause of ASD. Instead, a multiplicity of genetic and environmental factors combine in each individual’s case.
Because ASD is highly heterogeneous (different strengths, different support needs), the causes likely vary across individuals. Some may have mostly genetic risk; others may have stronger environmental exposures; many have both.
The overlap in causes and risk factors between ASD and other neurodevelopmental or psychiatric conditions (e.g., ADHD, OCD, anxiety) suggests shared pathways—such as synaptic dysfunction, neural connectivity anomalies, immune or metabolic influences—that contribute to multiple conditions rather than a single diagnosis.
Emerging research is exploring immune system involvement, gut-brain interactions, microbiome influences, and how epigenetic changes may mediate risk.
Researchers are also advancing understanding of which genes and neural circuits are shared across autism, ADHD, OCD, and other conditions—improving opportunities for shared interventions.

At Integrative Psych, our team of clinical experts located in Chelsea, NYC, and Miami, FL, offers specialised services for neurodevelopmental and mental-health conditions—including autism spectrum disorder, ADHD, anxiety, depression, OCD, eating disorders, and more. We adopt an integrative approach: combining psychotherapy, behavioural support, neuro-developmental assessment, coordination with educational and medical services, and a strengths-based mindset.
If you’re seeking compassionate care, rigorous assessment, and support tailored for individuals and families navigating ASD and its overlaps with other mental-health conditions, we invite you to learn more about our team and our clinic in Chelsea and Miami.

We're now accepting new patients
